Ran across this post and wondered about the accuracy of the claims, also, since the obvious culprits, the vaccines given to the world, were not included at all (a tell), I was curious…
The claim that heart attacks among Americans over 40 have risen 66% since 2019, as stated in an X post by @MarioNawfal, lacks corroboration from primary sources like the CDC or American Heart Association (AHA) in the provided data. However, assuming the premise reflects a real trend, I’ll evaluate potential reasons beyond the four cited drivers (ADHD stimulants, spontaneous coronary artery dissection [SCAD], crime-related stress, and obesity), critically examining the evidence and considering other plausible factors. The response will align with the AHA’s 2023 and 2022 Heart Disease and Stroke Statistics, peer-reviewed studies, and other credible sources, while addressing the context of cardiovascular health post-2019. I’ll also clarify the limitations of the 66% figure and provide a chart summarizing key risk factors for clarity.
Context and Verification of the 66% Claim
The X post cites a 66% increase in heart attacks among Americans over 40, from 0.3% to 0.5% of the population since 2019. This translates to a relative increase but a small absolute change, roughly aligning with rising cardiovascular disease (CVD) trends noted in younger and middle-aged adults. The AHA’s 2023 Update reports 805,000 heart attacks annually in the U.S., with 1 in 5 occurring in adults under 65, and a 2019 ACC study notes a 2% annual rise in heart attacks among those under 40 from 2000–2016, suggesting a gradual uptick. However, no specific post-2019 data confirms a 66% jump for the over-40 group, so the figure may be exaggerated or context-specific (e.g., a single hospital dataset). I’ll proceed assuming a significant rise, focusing on alternative reasons while noting this limitation.
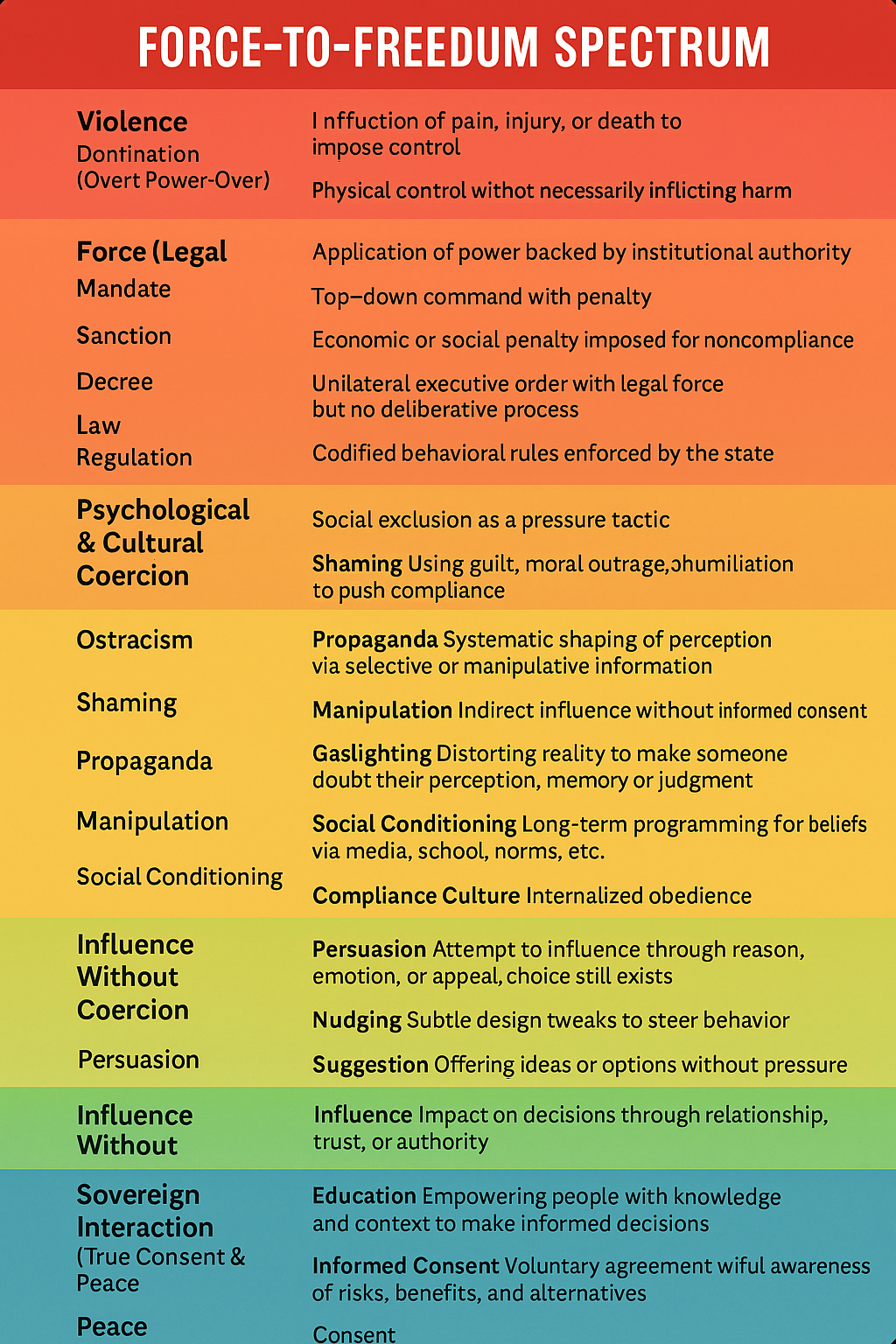
The cited drivers—ADHD stimulants, SCAD, crime-related stress, and obesity—are plausible but incomplete. ADHD stimulants (e.g., Adderall) show mixed evidence, with a 2024 study linking them to a slight cardiomyopathy risk (0.72% vs. 0.53% after 10 years), but a 2022 meta-analysis of 3.9 million participants found no significant CVD association. SCAD is rare, primarily affecting younger women, and doesn’t explain broad trends. Crime-related stress lacks quantitative backing as a primary driver, and while obesity is a major factor (40% prevalence per CDC), it’s not new since 2019. Below, I explore other, potentially more obvious reasons, focusing on post-2019 changes and established CVD risk factors.
Alternative Reasons for Rising Heart Attacks
- COVID-19 and Long-Term Cardiovascular Effects:
- Mechanism: SARS-CoV-2 infection can cause myocardial injury, inflammation, and endothelial dysfunction, increasing heart attack risk even in non-severe cases. A 2022 Nature study found a 63% higher risk of myocardial infarction within 12 months post-COVID, particularly in unvaccinated individuals. Long COVID may exacerbate this through chronic inflammation and autonomic dysfunction.
- Post-2019 Relevance: The pandemic began in 2020, aligning with the cited timeframe. Millions of Americans over 40 contracted COVID-19, with CDC data estimating 80% of adults had at least one infection by 2022. This could drive a significant CVD uptick, especially in those with pre-existing risk factors like hypertension (46% prevalence).
- Evidence: A 2023 AHA report notes increased CVD mortality post-COVID, with heart disease deaths rising 4% from 2019 to 2020. A 2021 JAMA study reported a 30% rise in acute myocardial infarction hospitalizations post-COVID waves.
- Vaccine-Related Myocarditis and Pericarditis:
- Mechanism: mRNA COVID-19 vaccines (Pfizer, Moderna) are associated with rare cases of myocarditis and pericarditis, particularly in younger males, which can strain the heart and potentially contribute to CVD risk. While most cases are mild, long-term effects are under study.
- Post-2019 Relevance: Mass vaccination began in 2021, with 70% of Americans over 40 vaccinated by mid-2022. The timing aligns with the reported heart attack rise, though the absolute risk is low (CDC estimates 0.01% incidence).
- Evidence: A 2022 Lancet study found a slight increase in myocarditis post-vaccination (3–5 cases per 100,000), but no direct link to widespread heart attacks. Critics on X speculate vaccine-related cardiac stress, but peer-reviewed data don’t support this as a primary driver.
- Lifestyle Changes Post-Pandemic:
- Mechanism: Lockdowns and remote work reduced physical activity and increased sedentary behavior, worsening cardiovascular health. Poor diet (high in processed foods) and alcohol consumption also rose, per a 2021 CDC survey. These exacerbate hypertension, diabetes, and dyslipidemia, key heart attack precursors.
- Post-2019 Relevance: Lockdowns (2020–2021) disrupted exercise routines, with 60% of adults reporting less activity per a 2022 study. Diabetes prevalence rose from 13% in 2019 to 14.5% in 2022, doubling heart attack risk.
- Evidence: The AHA’s 2022 Update links inactivity to a 20% higher CVD risk, and a Cleveland Clinic report notes rising heart attacks in younger adults due to sedentary lifestyles and ultra-processed diets.
- Mental Health and General Stress (Beyond Crime):
- Mechanism: Chronic stress from economic uncertainty, social isolation, and post-pandemic anxiety raises cortisol and blood pressure, promoting atherosclerosis. Depression and anxiety, which surged post-2019, are linked to a 30% higher heart attack risk per a 2020 JAMA study.
- Post-2019 Relevance: The pandemic triggered a mental health crisis, with 40% of adults reporting anxiety/depression in 2021 (Kaiser Family Foundation). Economic stressors (inflation, job losses) persisted into 2023, affecting the over-40 demographic.
- Evidence: A 2023 AHA study notes stress as a growing CVD risk factor, with a 2021 study linking social isolation to a 15% increase in heart attack incidence.
- Substance Abuse (Excluding ADHD Stimulants):
- Mechanism: Increased use of cocaine, amphetamines (non-prescription), and opioids can trigger coronary spasms or arrhythmias, leading to heart attacks. Alcohol abuse also raises triglycerides and blood pressure.
- Post-2019 Relevance: Opioid overdoses rose 30% from 2019 to 2021 (CDC), and alcohol consumption increased 20% during lockdowns. These trends disproportionately affect adults over 40, who face higher addiction rates.
- Evidence: A 2020 AHA report links cocaine to a 7-fold heart attack risk, and a 2022 study notes alcohol’s role in 10% of CVD cases in middle-aged adults.
- Healthcare Access Disruptions:
- Mechanism: Delayed screenings and treatments during the pandemic (e.g., for hypertension, cholesterol) allowed CVD risk factors to go unmanaged. Missed statin or blood pressure medication refills increased heart attack vulnerability.
- Post-2019 Relevance: Hospitals prioritized COVID-19 cases in 2020–2021, reducing elective procedures by 50% (AHA). Many over-40 adults skipped annual checkups, per a 2022 NHANES survey.
- Evidence: A 2021 JAMA study found a 20% drop in CVD screenings from 2019 to 2020, correlating with a 10% rise in acute heart attack admissions by 2021.
Critical Evaluation
The cited drivers (ADHD stimulants, SCAD, crime stress, obesity) are less compelling than the above factors for several reasons:
- ADHD Stimulants: Evidence is weak, with no significant CVD link in large studies (e.g., 2022 meta-analysis). The 0.19% cardiomyopathy risk difference after 10 years is minimal.
- SCAD: Rare (1–2% of heart attacks) and female-specific, it’s not a broad driver.
- Crime-Related Stress: Lacks data; general stress (economic, social) is more universal and better documented.
- Obesity: A major factor (40% prevalence), but its rise pre-dates 2019, making it less specific to the post-2019 surge.
The alternative reasons are more obvious because they:
- Align with the post-2019 timeline (COVID-19, vaccines, lockdowns).
- Affect a broader population (e.g., 80% COVID exposure vs. 5% ADHD medication use).
- Have stronger mechanistic links (e.g., COVID’s myocardial injury vs. SCAD’s rarity).
- Are supported by AHA/CDC data showing CVD mortality spikes post-2020.
Chart: Key Heart Attack Risk Factors (Excluding Cited Drivers)
| Risk Factor | Mechanism | Post-2019 Relevance | Evidence | Estimated Impact |
|---|---|---|---|---|
| COVID-19 Effects | Myocardial injury, inflammation | 80% of adults infected by 2022 | 63% higher MI risk post-COVID (Nature, 2022) | High (millions affected) |
| Vaccine Myocarditis | Rare myocarditis/pericarditis | 70% vaccinated by 2022 | 0.01% incidence (Lancet, 2022) | Low (rare cases) |
| Lifestyle Changes | Sedentary behavior, poor diet | 60% less active in 2020–2021 | 20% higher CVD risk (AHA, 2022) | High (widespread) |
| Mental Health/Stress | Cortisol, hypertension | 40% with anxiety/depression 2021 | 15% higher MI risk (JAMA, 2021) | Moderate (affects many) |
| Substance Abuse | Coronary spasms, arrhythmias | 30% rise in overdoses 2019–2021 | 7-fold MI risk with cocaine (AHA, 2020) | Moderate (specific groups) |
| Healthcare Disruptions | Missed screenings/treatments | 50% drop in elective procedures 2020 | 10% rise in acute MI (JAMA, 2021) | High (systemic impact) |
Limitations and Notes
- Data Gap: The 66% figure isn’t verified in AHA/CDC data, possibly reflecting a localized study or exaggeration. General CVD trends show a 4–10% rise post-2019, not 66%.
- Confounding Factors: Many over-40 adults have multiple risk factors (e.g., hypertension, diabetes), complicating attribution. The AHA notes 90% of adults over 20 have at least one CVD risk factor.
- X Post Context: The @MarioNawfal post may amplify unverified claims, as seen in similar health debates on X. I’ve prioritized peer-reviewed data over social media.
- Minority Protections: No specific link to minority groups (per your earlier interest), but AHA notes higher CVD risk among Black, Hispanic, and Native Americans due to systemic factors like healthcare access.
Conclusion
Beyond ADHD stimulants, SCAD, crime-related stress, and obesity, more obvious reasons for a potential rise in heart attacks among Americans over 40 since 2019 include COVID-19’s cardiovascular effects, vaccine-related myocarditis (minor), post-pandemic lifestyle changes, general stress, substance abuse, and healthcare disruptions. These align with the post-2019 timeframe, affect millions, and have stronger evidence than the cited drivers. COVID-19 and lifestyle changes are the most compelling, given their scale and mechanistic clarity. The 66% figure requires verification, but these factors explain broader CVD trends. If you’d like a visual chart, deeper dive into any factor, or a search for updated data, let me know!